YO Clinical Case: Mysterious vision loss in a teenager

Matteo Forlini MD
Retina Specialist and Vitreoretinal Surgeon (Italy)
Vitreoretinal Consultant at San Marino State Hospital (Republic of San Marino)
A 14 year old patient presented with sudden vision loss in the right eye. There was a central negative scotoma in his right eye for 10 days.
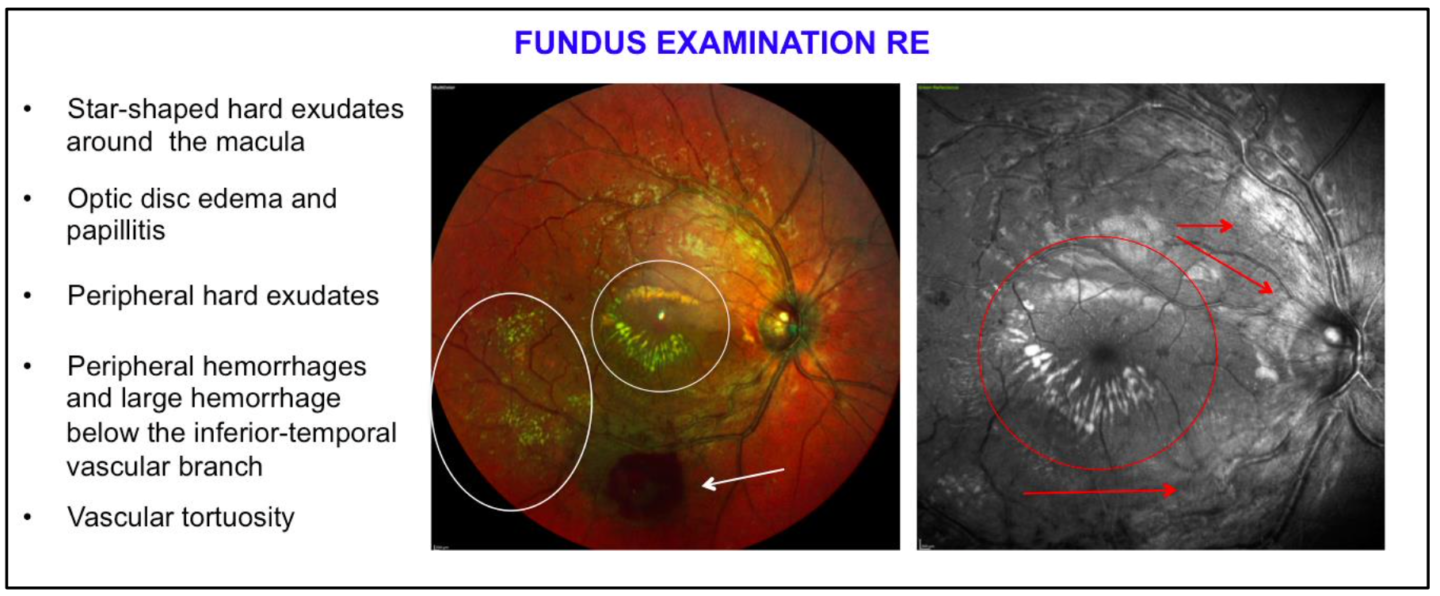
Examination revealed:
VOD: Count fingers at 50 cm
VOS: 20/20
Slit lamp examination OO: negative
Pupils: isochoric, isocyclic and reactive to light. Direct and consensual pupillary light reflexes were regular and there were no abnormalities found in ocular motility and convergence
IOP OO: 14 mmHg (pneumotonometry)
The differential diagnoses were:
– Coats’ disease: occurs at an earlier age
– Cat-scratch disease: the patient has a cat and reports that he was scratched a few weeks prior to the vision loss
– Other infectious neuroretinites: Syphilis, lyme disease, rocky mountain spotted fever, toxoplasmosis, toxocariasis, histoplasmosis, and leptospirosis
– Retinal vasculitis (infectious or autoimmune diseases)
– Retinal macroaneurysm: not associated with papillitis and vasculitis
– Eales disease: occurs at an older age; absence of papillitis
Further information:
Cat-scratch disease
Blood tests: negative
Bartonella henselae: absence of antibodies and general symptoms (lymphadenopathy, fever, decreased appetite, headache, chills, muscular pains)
Other infectious diseases
Blood tests: negative for antibodies against syphilis, cytomegalovirus, toxoplasmosis, tuberculosis, borrelia, HIV etc.
Antibodies against Epstein Barr Virus were found.
Retinal vasculitis
- Urinalysis: presence of glycosuria, increased creatinuria, potassium and magnesium
- Suspected retinitis from autoimmune interstitial tubular nephritis
- Nephrological visit: negative
- Autoantibodies for autoimmune diseases: negative (Anti-DNA, ANCA, ANA, FR, AMA, ENA, PCR)
No signs of vitritis
While awaiting fluorangiography, empirical therapy for an Epstein Barr Virus infection was started in association with corticosteroid therapy to reduce retinal and optic disk inflammation:
– Acyclovir 400 mg 3 times per day
– Prednisone 1 mg/kg
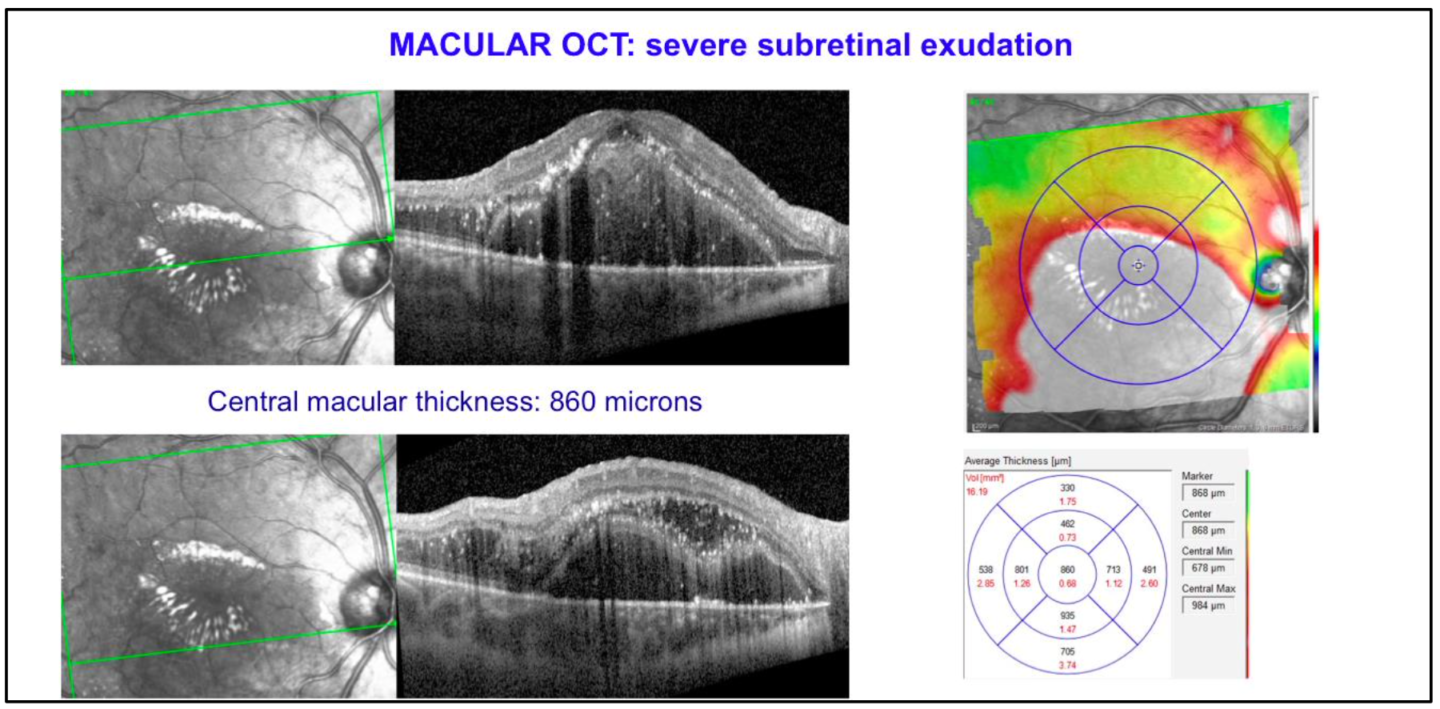
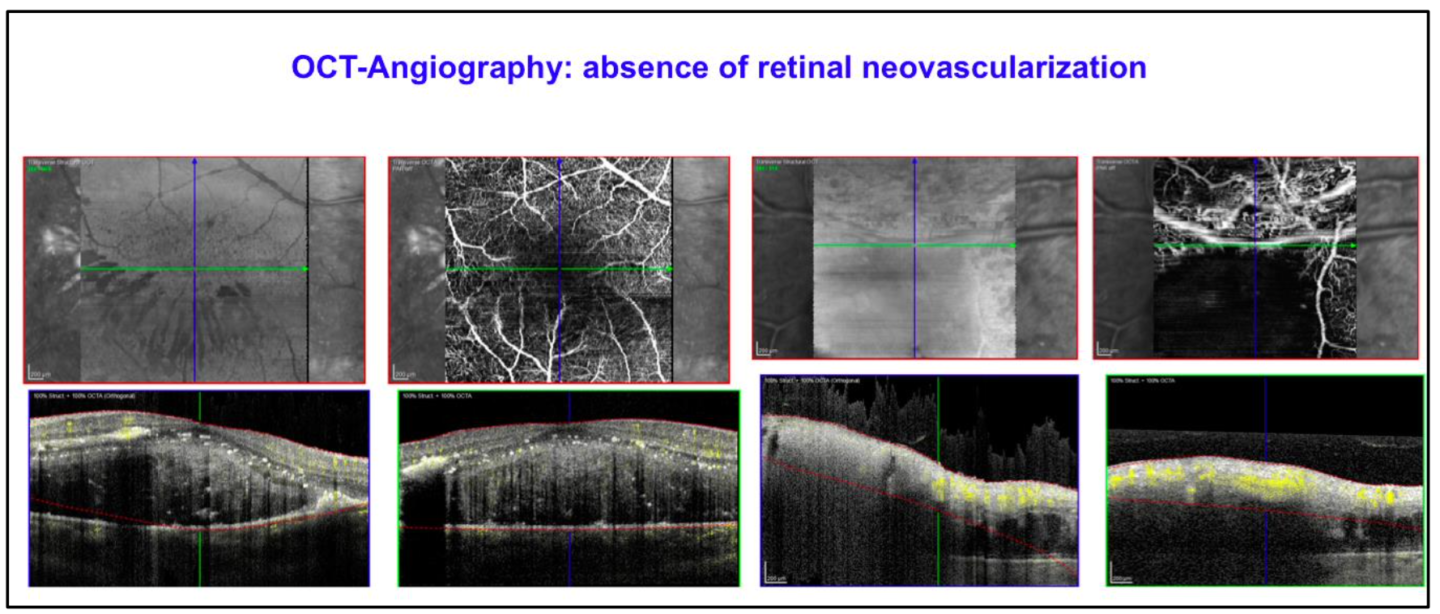
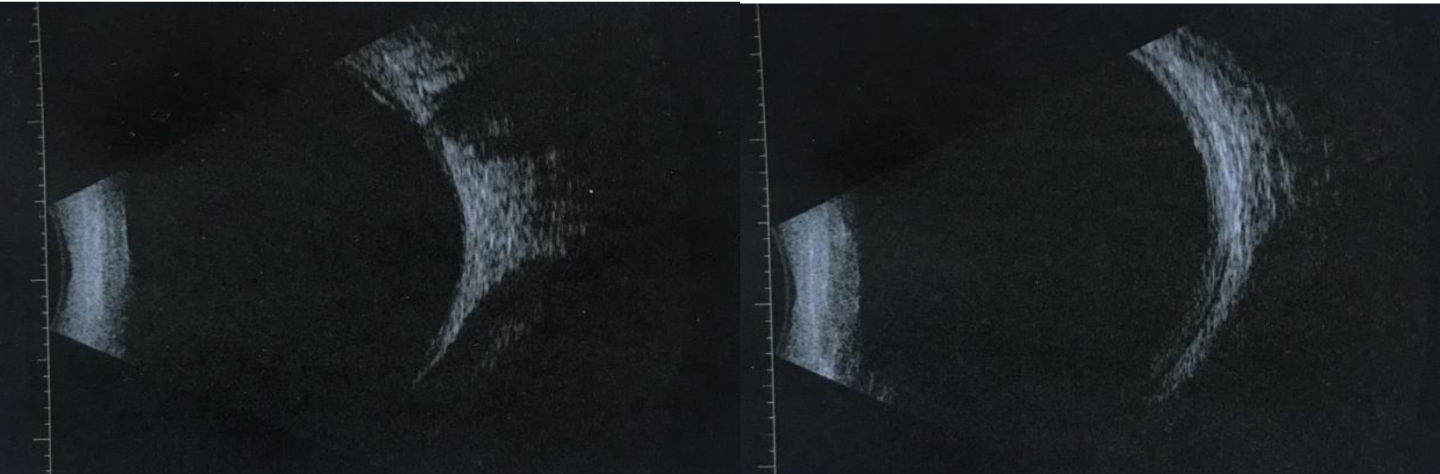
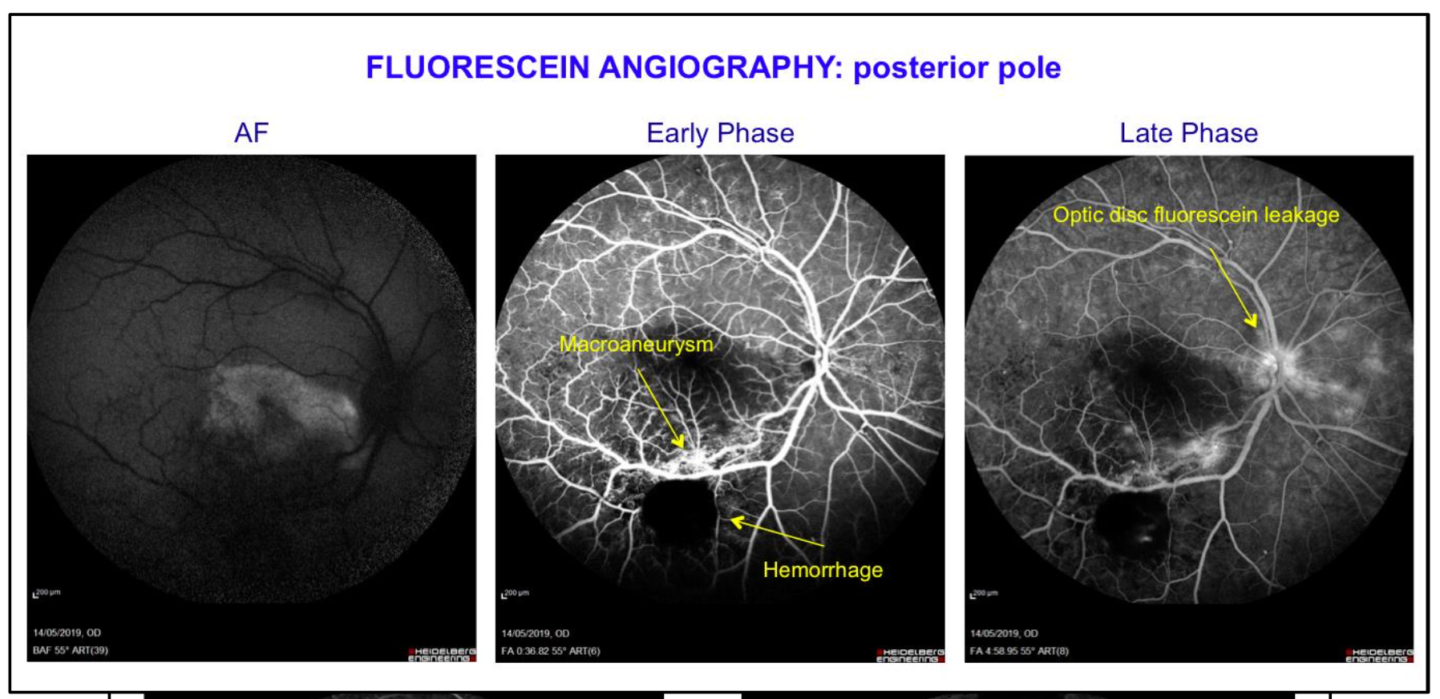
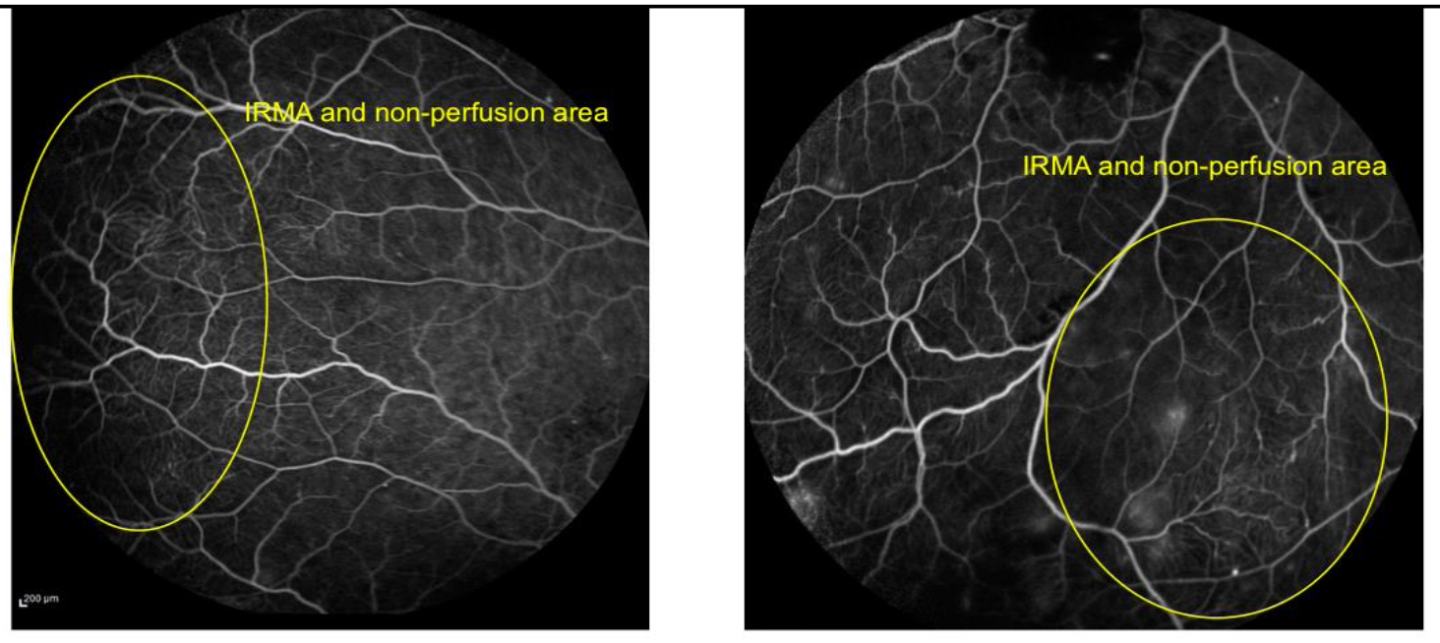
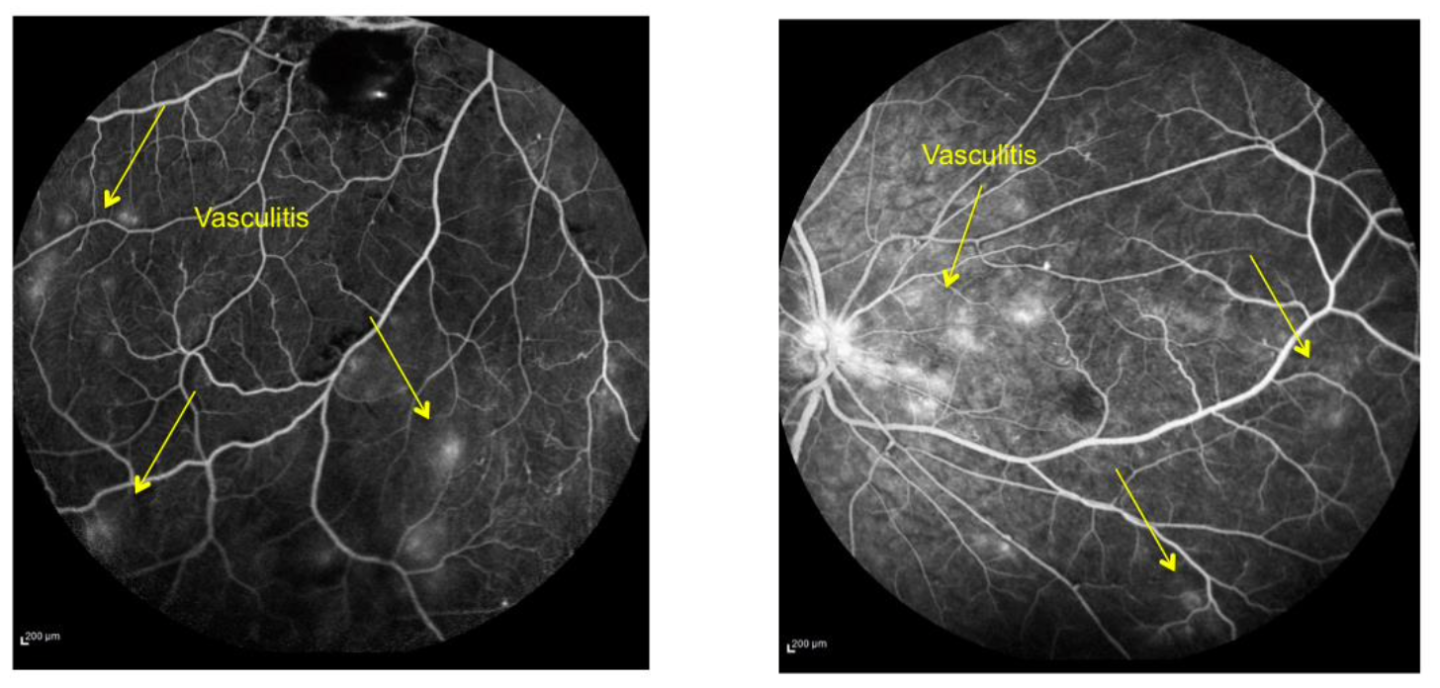
Fluorescein Angiography showed neuroretinitis, retinal macroaneurysm with exudation, vasculitis, IRMA and ischemia in peripheral vessels.
A diagnosis of exclusion was made:
Idiopathic Retinal Vasculitis, Aneurysms and Neuroretinitis Syndrome (IRVAN)
IRVAN
- First defined in 1983 by Kincaid and Schatz
- Unknown etiology
- Three major fundus findings: multiple aneurysmal dilatations, retinal vasculitis and neuroretinitis in arterial bifurcation
- Three minor fundus findings: peripheral capillary perfusion disorder, retinal neovascularization and macular exudation
- Very rare disorder that is seen in young people
- Diagnosis of exclusion with no specific tests
Karasu B et al. The fluorescein angiographic photodiagnosis of idiopathic retinal vasculitis, aneurysms, and neuroretinitis (IRVAN) syndrome: Outcome of combined therapy. Photodiagnosis Photodyn Ther. 2019
Chong YJ et al. Idiopathic retinal vasculitis, aneurysms and neuroretinitis (IRVAN): case series of three patients with multimodal imaging. Graefes Arch Clin Exp Ophthalmol. 2019
TREATMENT
- Oral therapy with Prednisone 1 mg/kg
- Intravitreal Dexamethasone Implant combined with an Aflibercept Injection in the same session – First therapy
- Focal laser treatment to the macroaneurysm – 2 weeks after the Dexamethasone Implant
- Sub-threshold micropulse laser treatment to the macula – 2 weeks after the Dexamethasone Implant (in the same session as focal laser treatment)
- Panretinal Photocoagulation to the peripheral areas of non perfusion – one month after the Dexamethasone Implant
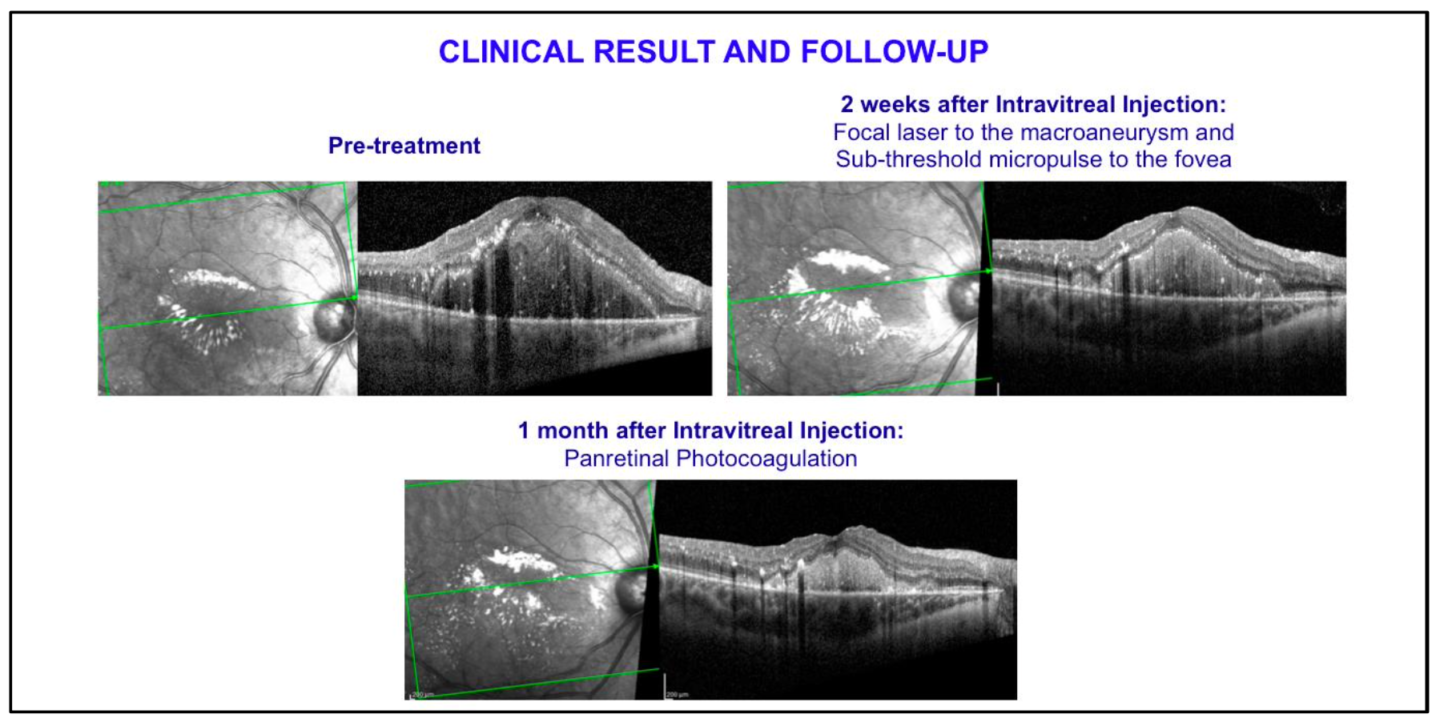
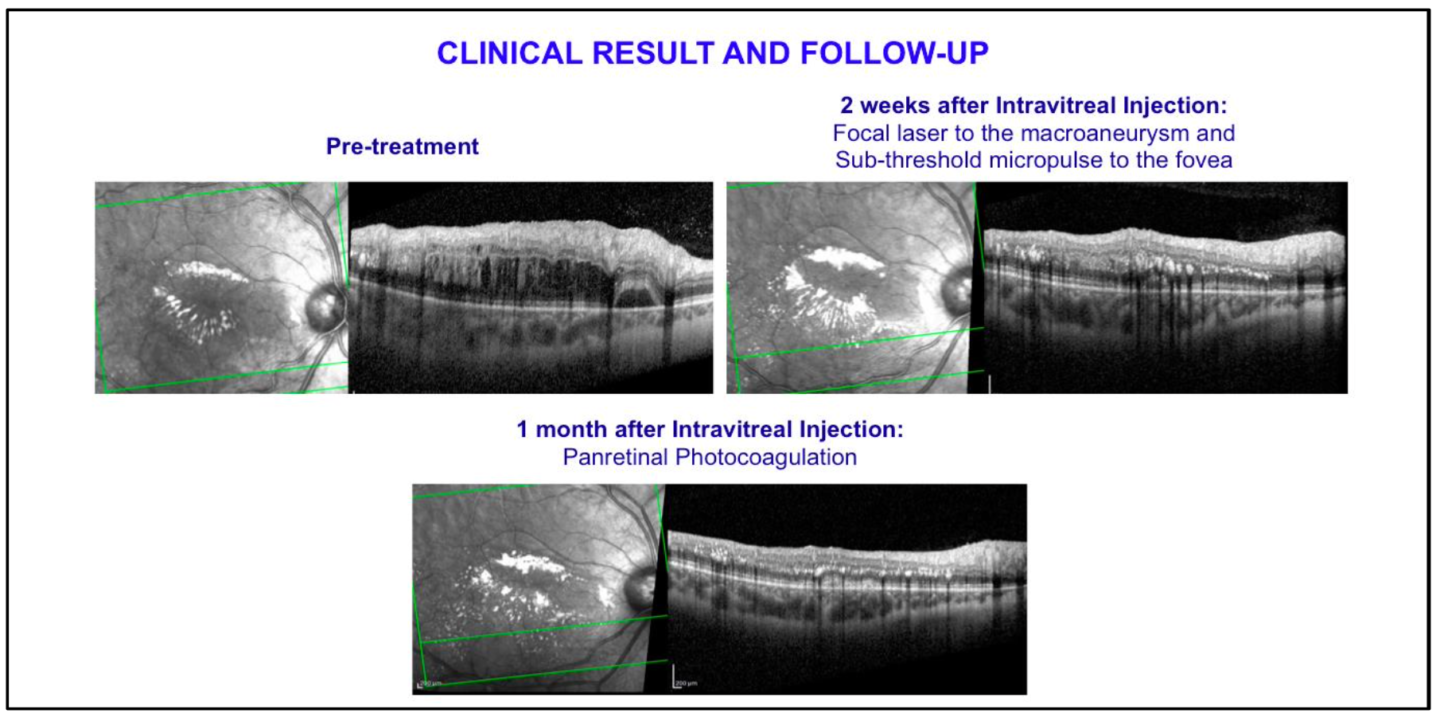
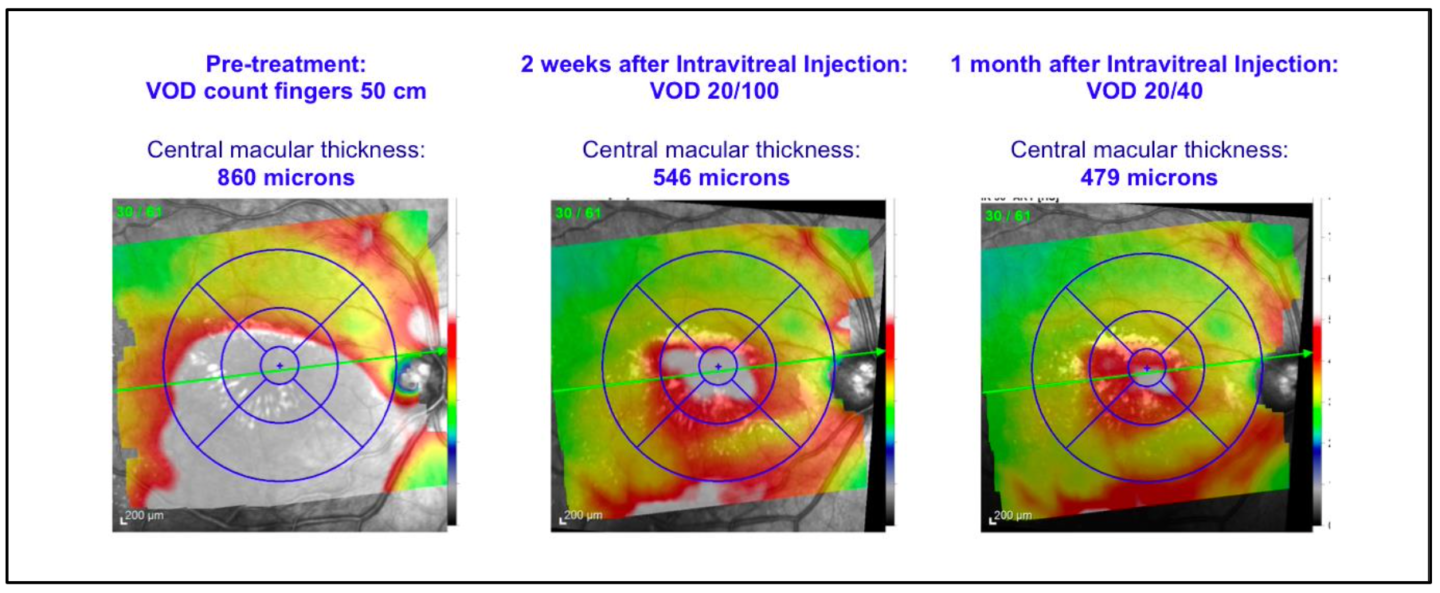
At the latest follow-up the patient presented BCVA 20/40 in the right eye, with a central macular thickness of 464 microns at OCT scan
No side effects were noted except a mild IOP rise treated with topical therapy.
CONCLUSION
- IRVAN is a diagnosis of exclusion with no specific tests
- The progression of IRVAN can vary greatly, despite aggressive treatment with PRP, intravitreal steroids and anti-VEGF agents
- The therapeutic approach must be customized based on the severity of the clinical findings: Intravitreal Dexamethasone Implant is effective in treating retinitis, papillitis and inflammatory exudation
- Multiple imaging modalities including Fluorescein angiography, OCT and OCT-angiography provide valuable information for disease monitoring and progression
- In our case, the patient will undergo a new Intravitreal Dexamethasone Implant
