YO Clinic Part II
In part two of the series, Jelena Potic (Serbia), who is a Fellow in Surgical Retina and Ocular Oncology at the Hôpital Ophtalmique Jules-Gonin, Switzerland, discusses important diagnoses not to miss: uveal melanoma.
Most Common Adult Ocular Tumour: Uveal Melanoma
Uveal melanoma represents the most common primary
malignant intraocular tumour, occurring most commonly in
adults aged about 60 years old. It is very rare in young people.
The global incidence of uveal melanoma is estimated to be 4.3
per million, men are more at risk (M:F 4.9 per million : 3.7 per
million). The choroid and iris are most commonly involved.
Melanoma is a malignant tumour arising from melanocytes,
which are present in uvea, conjunctiva, and skin. The important
predisposing factors fair skin, brighter iris colour, presence of
many cutaneous naevi, especially with atypical appearance,
uveal naevi or melanocytoma, and naevus of Ota.

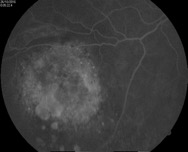
Fig. 1. Choroidal melanoma
Choroidal melanoma
About 80-90% of all uveal melanomas originate in choroid. In the early stage these tumours are asymptomatic. Patients may report non-specific symptoms, such as photopsia, floaters and metamorphopsia. In more advanced stages, there may be blurred vision or pain. Typically, these tumours are discovered on routine ophthalmological examination.
Fig. 2. Small choroidal melanoma without rupture of Bruch’s membrane, fluorescein angiography (A) and ultrasound biomicroscopy (B)
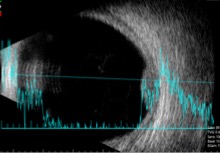
Fig. 2 B
The typical shape of choroidal melanoma is visible on ultrasound biomicroscopy (UBM): if Bruch’s membrane is still intact the tumour is dome-shaped, if there is a rupture of Bruch’s membrane at the apex the tumour is mushroom-shaped, or if Bruch’s membrane rupture is present at the border of the tumour, the tumour has an irregular configuration. Choroidal melanomas are usually grey-greenish-brown with orange pigment, but they can also be amelanotic (no pigmentation). They are often followed by secondary exudative retinal detachment. In advanced cases, there is secondary glaucoma or inflammatory reaction. Specific attention should be payed to the extrascleral extension of the tumour, though this is very rare.
Iris melanoma
About 8% of all melanomas originate from the iris. Typically, iris melanoma presents in middle age, several years prior to choroidal melanoma. Iris melanoma may be circumscribed or diffuse. They appear most frequently in the inferior iris but can be located elsewhere.
Unless tumour growth is noted by the patient, iris melanoma usually are asymptomatic in presentation. However, vision loss could occur in advanced stages due to cataract, hyphaema, corneal decompensation, seeding in the anterior chamber, or secondary glaucoma.
Usually, these patients already had a history of iris naevus that is under regular review. Malignant transformation occurs in about 8% over 15 years. The key features include tumour growth and the appearance of new blood vessels on the tumour surface.
Tumour growth is typically slow but can lead to corectopia and/or ciliary body invasion. It is important to perform a detailed clinical examination, including slit lamp examination, gonioscopy, and UBM.
Ciliary body melanoma
Ciliary melanoma is the rarest among the uveal melanomas. Similar to other uveal melanomas, in the early stages, the ciliary body tumour is asymptomatic.
They can be circumscribed or in a ring-shaped (annular) formation. The circumscribed type is usually brown and nodular. They may seed into the anterior chamber, or around the ciliary body. Annular melanoma should be suspected in presence of sentinel vessels on the external sclera, sectoral iris neovascularization, irregular shallowing of anterior chamber, and iridocyclitis.
Detailed clinical evaluation is essential in diagnosis, including slit lamp examination with and without transillumination, gonioscopy, and UBM. Cyst formation on UBM is a poor prognostic sign.
Differential Diagnosis
Iris and ciliary body melanomas can be confused with iris naevi, iris metastasis, Cogan-Reese syndorme, Iris stromal cyst, melanocytoma.
Differential diagnoses of choroidal melanoma include choroidal naevus, choroidal metastasis, choroidal hemangioma and other choroidal lesions that might be similar, such as involutional macular degeneration, ruptured arteriolar macroaneurysm, choroidal hemorrhage, hemorrhagic retinal detachment etc.
Very commonly employed to distinguish choroidal naevi from choroidal melanoma is the useful mnemonic developed by Carol Shields and coauthors: “To Find Small Ocular Melanoma Using Helpful Hints Daily” (TFSON-UHHD):
| T | Thickness >2mm |
| F | subretinal Fluid |
| S | Symptoms (photopsia, decreased visual acuity etc) |
| O | Orange pigment present (intracellular lipofuscin) |
| M | Margin of tumour (within 3mm of the optic disc) |
| UH | Ultrasonographic Hollowness |
| H | absence of Halo (circular band of depigmentation) |
| D | absence of Drusen |